Tissue Engineers Are Currently Using Stem Cells To Repair What Type Of Tissue?
- What are tissue engineering and regenerative medicine?
- How do tissue engineering and regenerative medicine piece of work?
- How do tissue engineering and regenerative medicine fit in with current medical practices?
- What are NIH-funded researchers developing in the areas of tissue engineering and regenerative medicine?
What are tissue engineering and regenerative medicine?
Tissue applied science evolved from the field of biomaterials development and refers to the exercise of combining scaffolds, cells, and biologically active molecules into functional tissues. The goal of tissue engineering is to gather functional constructs that restore, maintain, or improve damaged tissues or whole organs. Bogus skin and cartilage are examples of engineered tissues that have been approved by the FDA; yet, currently they have express use in human patients.
Regenerative medicine is a broad field that includes tissue applied science but also incorporates research on self-healing – where the body uses its ain systems, sometimes with assist foreign biological material to recreate cells and rebuild tissues and organs. The terms "tissue engineering science" and "regenerative medicine" accept become largely interchangeable, as the field hopes to focus on cures instead of treatments for complex, often chronic, diseases.
This field continues to evolve. In add-on to medical applications, non-therapeutic applications include using tissues as biosensors to detect biological or chemical threat agents, and tissue chips that can be used to test the toxicity of an experimental medication.
How exercise tissue engineering science and regenerative medicine work?
Cells are the building blocks of tissue, and tissues are the basic unit of function in the torso. Generally, groups of cells make and secrete their own back up structures, called extra-cellular matrix. This matrix, or scaffold, does more than just support the cells; information technology also acts as a relay station for various signaling molecules. Thus, cells receive messages from many sources that become bachelor from the local environment. Each signal can start a chain of responses that determine what happens to the cell. By understanding how individual cells answer to signals, interact with their environment, and organize into tissues and organisms, researchers have been able to dispense these processes to mend damaged tissues or even create new ones.
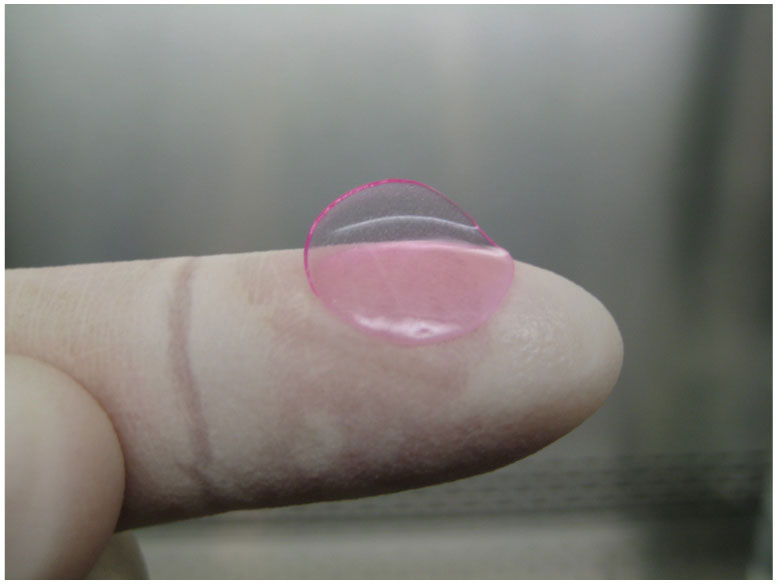
The procedure ofttimes begins with building a scaffold from a wide set of possible sources, from proteins to plastics. One time scaffolds are created, cells with or without a "cocktail" of growth factors tin can be introduced. If the environment is correct, a tissue develops. In some cases, the cells, scaffolds, and growth factors are all mixed together at once, allowing the tissue to "cocky-assemble."
Some other method to create new tissue uses an existing scaffold. The cells of a donor organ are stripped and the remaining collagen scaffold is used to abound new tissue. This procedure has been used to bioengineer middle, liver, lung, and kidney tissue. This arroyo holds bully promise for using scaffolding from human tissue discarded during surgery and combining information technology with a patient's own cells to make customized organs that would not be rejected by the immune organisation.
How do tissue engineering and regenerative medicine fit in with current medical practices?

Source: Stephen Badylak, University of Pittsburgh.
Currently, tissue engineering science plays a relatively pocket-sized role in patient handling. Supplemental bladders, modest arteries, skin grafts, cartilage, and even a full trachea have been implanted in patients, merely the procedures are withal experimental and very costly. While more complex organ tissues similar eye, lung, and liver tissue accept been successfully recreated in the lab, they are a long manner from existence fully reproducible and ready to implant into a patient. These tissues, even so, can exist quite useful in inquiry, especially in drug evolution. Using functioning man tissue to aid screen medication candidates could speed upwardly development and provide central tools for facilitating personalized medicine while saving money and reducing the number of animals used for research.
What are NIH-funded researchers developing in the areas of tissue technology and regenerative medicine?
Research supported by NIBIB includes evolution of new scaffold materials and new tools to fabricate, image, monitor, and preserve engineered tissues. Some examples of enquiry in this area are described below.
- Controlling stem cells through their environment:
For many years, scientists have searched for ways to control how stems cells develop into other jail cell types, in the hopes of creating new therapies. Two NIBIB researchers accept grown pluripotent cells—stem cells that have the ability to turn into whatever kind of jail cell—in different types of defined spaces and constitute that this confinement triggered very specific gene networks that determined the ultimate fate for the cells. Most other medical research on pluripotent stem cells has focused on modifying the combination of growth solutions in which the cells are placed. The discovery that there is a biomechanical chemical element to decision-making how stem cells transform into other prison cell types is an important slice of the puzzle as scientists effort to harness stems cells for medical uses.
- Implanting human livers in mice:
NIBIB-funded researchers accept engineered human liver tissue that can exist implanted in a mouse. The mouse retains its ain liver too, and therefore its normal function-but the added piece of engineered human being liver can metabolize drugs in the same way humans do. This allows researchers to examination susceptibility to toxicity and to demonstrate species-specific responses that typically do non evidence up until clinical trials. Using engineered human tissue in this mode could cut down on the time and toll of producing new drugs, as well as allow for critical examinations of drug-drug interactions within a human-similar arrangement. - Engineering mature os stalk cells:
Researchers funded past NIBIB completed the get-go published study that has been able to take stalk cells all the mode from their pluripotent state to mature bone grafts that could potentially exist transplanted into a patient. Previously, investigators could only differentiate the cells to a archaic version of the tissue which was not fully functional. Additionally, the written report found that when the bone was implanted in immunodeficient mice there were no aberrant growths afterwards—a problem that ofttimes occurs later on implanting stem cells or bone scaffolds alone. - Using lattices to help engineered tissue survive:
Currently, engineered tissues that are larger than 200 microns (near twice the width of a human pilus) in any dimension cannot survive considering they exercise non have vascular networks (veins or arteries). Tissues need a good "plumbing system"—a mode to bring nutrients to the cells and carry abroad the waste matter—and without a claret supply or similar mechanism, the cells quickly die. Ideally, scientists would like to be able to create engineered tissue with this plumbing arrangement already built in. I NIBIB funded researcher is working on a very elementary and easily reproducible system to solve this problem: a modified ink-jet printer that lays down a lattice made of a saccharide solution. This solution hardens and the engineered tissue (in a gel course) surrounds the lattice. Later, blood is added which easily dissolves the saccharide lattice, leaving pre-formed channels to act every bit claret vessels.
- New promise for the bum knee:
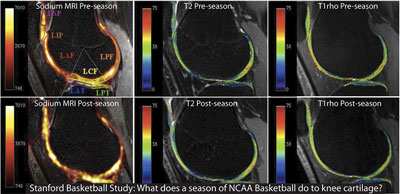
Until at present, cartilage has been very difficult, if not impossible, to repair due to the fact that cartilage lacks a blood supply to promote regeneration. There has been a 50% long-term success rate using microfracture surgery in young adults suffering from sports injuries, and little to no success in patients with widespread cartilage degeneration such every bit osteoarthritis. An NIBIB-funded tissue engineer has adult a biological gel that tin can exist injected into a cartilage defect following microfracture surgery to create an environs that facilitates regeneration. However, in order for this gel to stay in identify inside the knee, researchers also developed a new biological adhesive that is able to bond to both the gel as well as the damaged cartilage in the knee, keeping the newly regrown cartilage in identify. The gel/adhesive philharmonic was successful in regenerating cartilage tissue post-obit surgery in a recent clinical trial of fifteen patients, all of whom reported decreased pain at vi months post-surgery. In contrast, the bulk of microfracture patients, after an initial subtract in pain, returned to their original pain level within six months. This researcher worked in collaboration with another NIBIB grantee to image the patients who had undergone surgery enabling scientists to combine new, non-invasive methods to see the evolving results in real-fourth dimension. - Regenerating a new kidney:
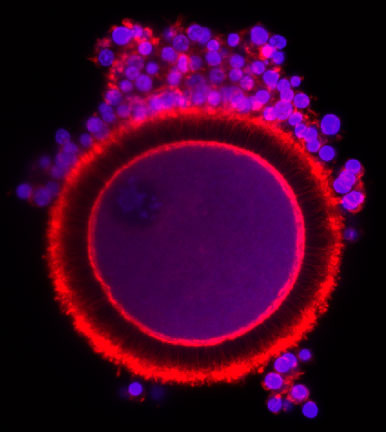
The ability to regenerate a new kidney from a patient's own cells would provide major relief for the hundreds of thousands of patients suffering from kidney disease. Experimenting on rat, pig and homo kidney cells, NIDDK supported researchers broke new ground on this front by first stripping cells from a donor organ and using the remaining collagen scaffold to help guide the growth of new tissue. To regenerate viable kidney tissue, researchers seeded the kidney scaffolds with epithelial and endothelial cells. The resulting organ tissue was able to articulate metabolites, reabsorb nutrients, and produce urine both in vitro and in vivo in rats. This process was previously used to bioengineer heart, liver, and lung tissue. The creation of transplantable tissue to permanently supersede kidney function is a leap forrard in overcoming the problems of donor organ shortages and the morbidity associated with immunosuppression in organ transplants.
Tissue Engineers Are Currently Using Stem Cells To Repair What Type Of Tissue?,
Source: https://www.nibib.nih.gov/science-education/science-topics/tissue-engineering-and-regenerative-medicine
Posted by: smithpule1960.blogspot.com


0 Response to "Tissue Engineers Are Currently Using Stem Cells To Repair What Type Of Tissue?"
Post a Comment